Peripheral Artery Disease (PAD and deep vein thrombosis (DVT) affect circulation in the lower extremities with blockages in the veins. PAD blocks arteries by plaque buildup, whereas blood clots cause DVT blockages.
Maintaining healthy blood vessels is key for overall well-being, ensuring efficient delivery of oxygen and nutrients to the body while preventing serious complications like strokes, heart disease, and mobility issues.
If you are experiencing symptoms of peripheral artery disease (PAD) or deep vein thrombosis (DVT), you should seek expert help immediately. For over 15 years, USA Vascular Centers have been offering minimally invasive treatments for PAD.
What is Peripheral Artery Disease (PAD)?
Peripheral Artery Disease (PAD) is a progressive vascular condition characterized by the narrowing of the arteries, most commonly those supplying blood to the legs and feet. This process gradually reduces blood flow, leading to a variety of symptoms and health complications.
The primary cause of PAD is atherosclerosis, a process where plaque builds up on the inner walls of the arteries. This plaque accumulation gradually obstructs blood flow, hindering the delivery of oxygen and nutrients to the lower extremities.
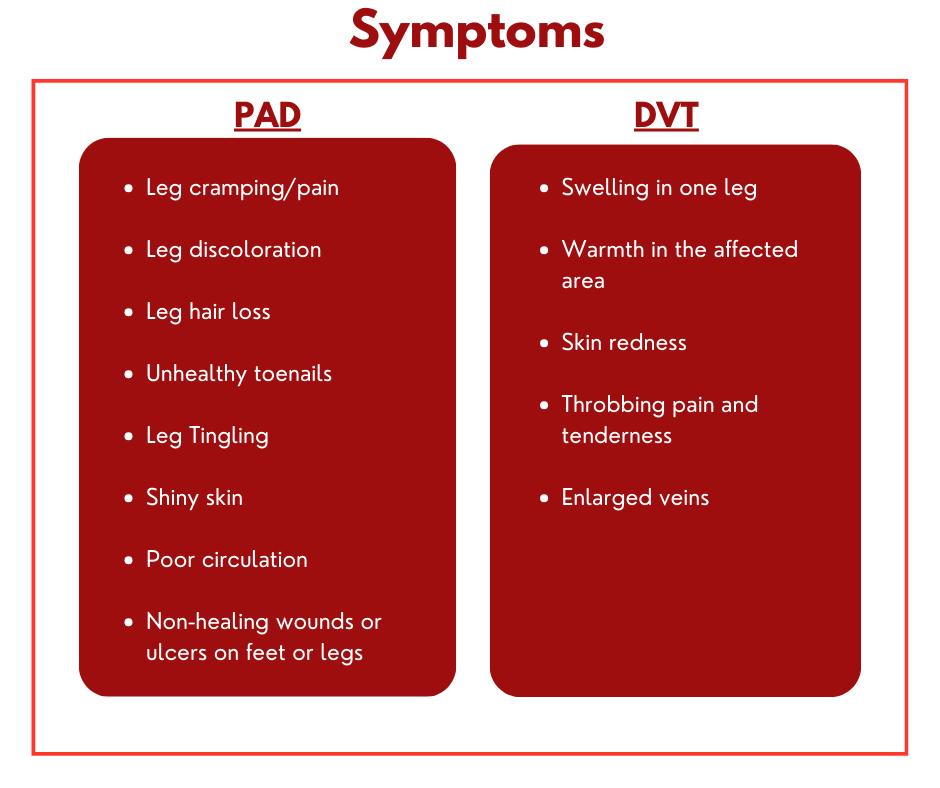
Common Symptoms of PAD include:
- Intermittent claudication: Cramping pain, aching, or fatigue in the muscles of the legs or hips during exercise, which subsides with rest.
- Numbness or coldness in the legs or feet compared to other parts of the body.
- Slow-healing sores or ulcers on the feet or toes
- Changes in skin color and shiny skin on the legs and feet.
- Hair loss on the legs and feet.
Smoking, diabetes, high blood pressure and cholesterol, and a family history of vascular disease are factors that can increase your risk of developing PAD.
What is Deep Vein Thrombosis (DVT)?
Deep Vein Thrombosis (DVT) is a medical condition characterized by a blood clot forming within a deep vein, most commonly in the legs. This blockage can restrict blood flow and potentially lead to severe complications.
The primary causes of DVT:
- Slowed Blood Flow (Venous Stasis): When blood flow in the veins is sluggish, it increases the likelihood of clot formation. This can occur due to prolonged immobility, such as during long flights, extended bed rest, or paralysis.
- Vein Damage (Endothelial Injury): Injury to the inner lining of a vein can trigger the clotting process. This damage can result from surgery, trauma, or certain medical conditions.
- Increased Blood Clotting (Hypercoagulability): Some individuals are predisposed to excessive blood clotting due to genetic factors or acquired conditions. Certain medications, like hormone replacement therapy or birth control pills, can also increase this risk.
Common symptoms of DVT include:
- Swelling in the affected leg.
- Pain or tenderness in the leg, often described as cramping or soreness.
- Warmth over the affected area.
- Red or discolored skin.
Several factors increase the risk of deep vein thrombosis (DVT), such as long periods of inactivity, recent surgery or injury, certain medical conditions like cancer or heart failure, and some medications such as hormone therapy or birth control pills. Additionally, having peripheral artery disease (PAD) can also elevate DVT risk.
PAD vs. DVT: Understanding Key Differences
While both (PAD) and (DVT) fall under the broader category of peripheral vascular disease and may share some common risk factors, they are distinct conditions affecting different parts of the circulatory system. Understanding their key differences is crucial for accurate diagnosis and timely intervention.
Type of Blood Vessel:
- PAD: Primarily affects the arteries, the vessels that carry oxygen-rich blood away from the heart to the limbs and organs.
- DVT: Occurs in the veins, the vessels that return deoxygenated blood back to the heart.
Cause:
- PAD: The primary cause is atherosclerosis, characterized by the buildup of plaque (fatty deposits) inside the arterial walls, leading to narrowing or blockage of the arteries.
- DVT: Results from the formation of a blood clot within a deep vein, typically in the legs.
Nature of Pain:
- PAD: Pain associated with PAD, known as claudication, occurs as cramping or aching in the legs or feet during exercise, which subsides with rest.
- DVT: Pain associated with DVT is usually constant, presenting as persistent aching, tenderness, and swelling in the affected limb, even at rest.
Temperature of Affected Area:
- PAD: The affected limb tends to be cold to the touch due to reduced blood flow.
- DVT: The affected area often feels warm due to inflammation and increased blood flow associated with the clot.
Skin Color Changes:
- PAD: Skin may appear pale, bluish, or shiny due to inadequate oxygen delivery.
- DVT: The skin may become red or discolored due to inflammation and blood congestion.
The Danger of Each Disease:
- PAD: Severe PAD can lead to critical limb ischemia (CLI), a condition characterized by severe blockage of the arteries, resulting in chronic rest pain, non-healing ulcers, and gangrene. This can lead to limb amputation. Furthermore, PAD is also associated with an increased risk of heart attack and stroke.
- DVT: The most serious complication of DVT is pulmonary embolism (PE). This occurs when a clot breaks loose and travels to the lungs, obstructing blood flow. PE is a life-threatening condition requiring immediate medical attention.
Can Peripheral Artery Disease Cause DVT?
While PAD doesn’t directly cause DVT, they can coexist due to shared risk factors such as older age, smoking, diabetes, high cholesterol, and inactivity. PAD is characterized by narrowed arteries, primarily in the legs, leading to symptoms such as leg pain during exercise (claudication), numbness, or weakness in the legs. People with PAD also have an underlying risk for blood clots that can cause serious blockages in the legs. This is because some plaques, in addition to reducing blood flow through the arteries, can rupture. A ruptured plaque triggers your body’s blood-clotting response.
This is where the development of deep vein thrombosis (DVT) comes in. DVT involves blood clots forming in deep veins, typically in the legs, and presents with symptoms such as swelling in the affected leg, pain or tenderness not caused by injury, warmth in the skin over the affected area, and redness or discoloration of the skin. These shared risk factors mean that an individual can experience symptoms of both conditions simultaneously.
Check If You Are At Risk For PAD
Tests and Diagnosis
PAD diagnosis typically involves non-invasive methods like the ankle-brachial index (ABI), which compares ankle and arm blood pressures to detect arterial narrowing, often followed by ultrasound, imaging such as angiography (using X-rays and contrast dye) for detailed visualization of blockages.
Similarly, DVT diagnosis relies on ultrasound to visualize clots, the D-dimer test to measure clot breakdown products, and, in some cases, venography (invasive X-ray with contrast) to provide detailed vein images. The D-dimer test measures a substance in the blood that is released when a clot dissolves; however, it is not specific to DVT and may be elevated in other conditions.
DVT Vs. PAD Treatments
Treatments for Peripheral Artery Disease
PAD requires treatment to alleviate symptoms and prevent the condition from progressing. Lifestyle changes, such as quitting smoking, regular exercise, and a healthy diet, need to be combined with minimally invasive treatment options to improve leg circulation. The treatment options available at USA Vascular Centers for PAD include the following:
- Angioplasty: A minimally invasive procedure where a balloon is inserted into the narrowed or blocked artery. The balloon is then inflated to press against the walls and widen the artery for increased blood flow.
- Stent placement: An expandable mesh stent (tube) is inserted into the affected artery. This procedure allows normal blood flow by widening the artery and preventing it from collapsing.
- Atherectomy: A minimally invasive procedure where a catheter is inserted in the blocked artery. The plaque buildup is then scraped or shaved away from the arterial walls, restoring or improving blood flow.
Minimally Invasive PAD Treatments
Treatments for Deep Vein Thrombosis (DVT)
DVT treatment focuses on preventing clots from growing and reducing the risk of pulmonary embolism. Anticoagulant medications, commonly known as blood thinners, are the cornerstone of DVT treatment. Compression stockings can help reduce swelling and improve blood flow in the legs. In certain circumstances, thrombolysis, a procedure to dissolve the clot using medications delivered directly into the affected vein, may be used.
DVT Vs. PAD Prevention
While PAD and DVT are both vascular health conditions, their causes and preventative measures differ significantly. With PAD, everyday modifications can help prevent the progression of the disease, such as maintaining healthy blood sugar levels through diet and exercise, controlling blood pressure and cholesterol with lifestyle changes or medication, and adopting a heart-healthy diet. Smoking severely worsens PAD by damaging blood vessels and increasing the risk of blockages, hindering blood flow to the limbs. If there’s a family history of PAD or heart disease, regular check-ups with a doctor are essential for early detection and intervention.
Preventative measures for DVT focus on regular movement to maintain blood flow, even small leg exercises during long periods of sitting. Compression stockings can also significantly reduce the risk by improving circulation in the legs, particularly for individuals at higher risk, such as those recovering from surgery or with limited mobility.
Vascular Disease Prevention Tips
Can You Have Both DVT and PAD?
Since PAD and DVT share risk factors and people with PAD are more likely to get DVT, both conditions need a complete vascular health management plan to reduce the incidence and progression of both PAD and DVT.
Patients with clogged leg arteries must be monitored closely for blood clots and other signs and symptoms of DVT, including unilateral leg pain, swelling, and warmth. Individuals diagnosed with DVT should undergo a thorough assessment for risk factors associated with PAD, such as smoking history, hypertension, and diabetes. The overlapping risk factors prove that the two vascular conditions can occur simultaneously.
When to Seek Medical Attention: USA Vascular Centers Is Here to Help
PVD and DVT can lead to severe complications, such as heart disease and pulmonary embolism. However, receiving treatment and managing these conditions can significantly improve outcomes.
Recognizing vascular issues early is key for effective treatment and disease progression. If you are experiencing PAD symptoms like leg pain or cramping during exercise, non-healing foot sores, or changes in skin color or temperature, or DVT symptoms like sudden leg swelling, pain, warmth, and redness, it is time to seek medical assistance.
USA Vascular Centers emphasizes the adoption of minimally invasive procedures. If you have any concerns about your vascular health, consult our specialists today for expert diagnosis and care.
USA Vascular Centers offers routine vascular screenings and personalized treatment plans for individuals who are at risk for PAD or have been diagnosed with PAD. For more information, schedule a consultation online or call us at 888.773.2193 today.
FAQS
Are DVT and PAD related?
Both PAD and DVT affect the circulatory system, meaning they involve problems with blood vessels. and may exhibit similar symptoms but have different causes and effects. Both conditions commonly manifest in the legs, although PAD can affect arteries in the arms.
Can I have both DVT and PAD at the same time?
Yes, it is possible, though not typical, to have both conditions together, depending on the level of your circulation and the severity of the symptoms. However, it’s important to remember the key differences. PAD is a disease of the arteries, causing reduced blood flow to the limbs. DVT is a disease of the veins involving a blood clot obstructing blood flow from the limbs.