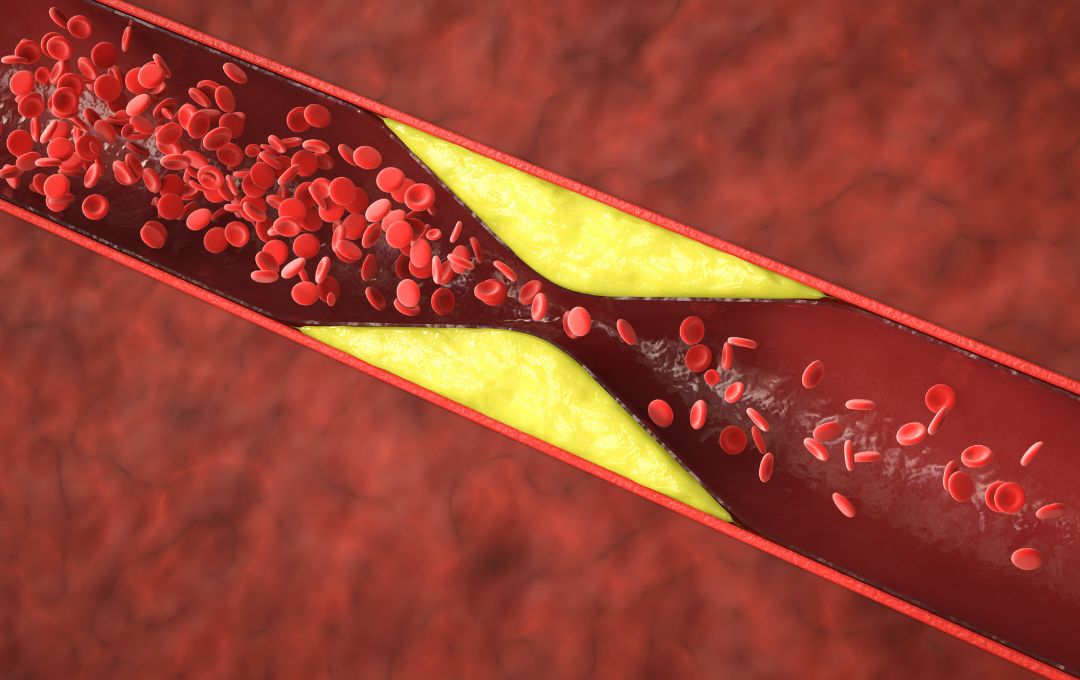
Peripheral artery disease (PAD) affects the arteries that supply blood to the lower extremities. Like the coronary arteries supplying the heart, these peripheral arteries can become clogged with plaque—a buildup of fat, cholesterol, calcium, and other substances. This plaque, known as atherosclerosis, narrows the arteries and restricts blood flow.
According to the National Library of Medicine, PAD can manifest in various ways: asymptomatic (no noticeable symptoms), symptomatic (causing pain or other issues), acute, or chronic.
PAD affects the legs, but atherosclerosis—the underlying cause—can occur in any artery, impacting the heart, brain, kidneys, and other vital organs. Because PAD can be problematic even when asymptomatic, vascular screenings are especially important for those with risk factors such as high blood pressure, diabetes, or high cholesterol.
Asymptomatic PAD
PAD is a progressive condition characterized by plaque buildup in the arteries that supply blood to the limbs, most commonly the legs. When PAD causes noticeable symptoms, such as leg pain during exercise, it can be diagnosed and treated.
Asymptomatic PAD is the “silent” form of PAD. This means you may have narrowed arteries in your legs or arms, leading to reduced blood flow, without experiencing pain, discomfort, or other typical PAD symptoms such as leg discoloration, shiny skin, non-healing wounds, and leg hair loss.
High blood pressure, high cholesterol, diabetes, and smoking put you at risk for asymptomatic PAD – without showing any warning signs. Regular vascular screenings are essential to keep a check.
PAD often presents asymptomatically at first, meaning patients may experience no leg symptoms. This “silent” nature of PAD makes awareness and monitoring of risk factors especially important.
Prevalence of PAD
PAD affects one in 20 Americans, particularly those over 50. While some experience leg pain during exercise, a significant portion (20% and 50%), are asymptomatic, making early diagnosis challenging, as individuals may not realize they have the condition until it progresses.
PAD prevalence increases with age and is more common in men. Many people with PAD also have coronary artery disease or diabetes, highlighting the interconnection between the underlying conditions.
Tests to Diagnose Asymptomatic Peripheral Artery Disease
PAD, whether symptomatic or asymptomatic, presents significant health risks. Therefore, early and accurate diagnosis is essential for effective management. Let’s explore standard diagnostic methods, from simple screenings to more advanced imaging. Here are a few methods of diagnosing PAD, ranging from simple screenings to advanced imaging techniques.
Ankle-Brachial Index to Detect PAD
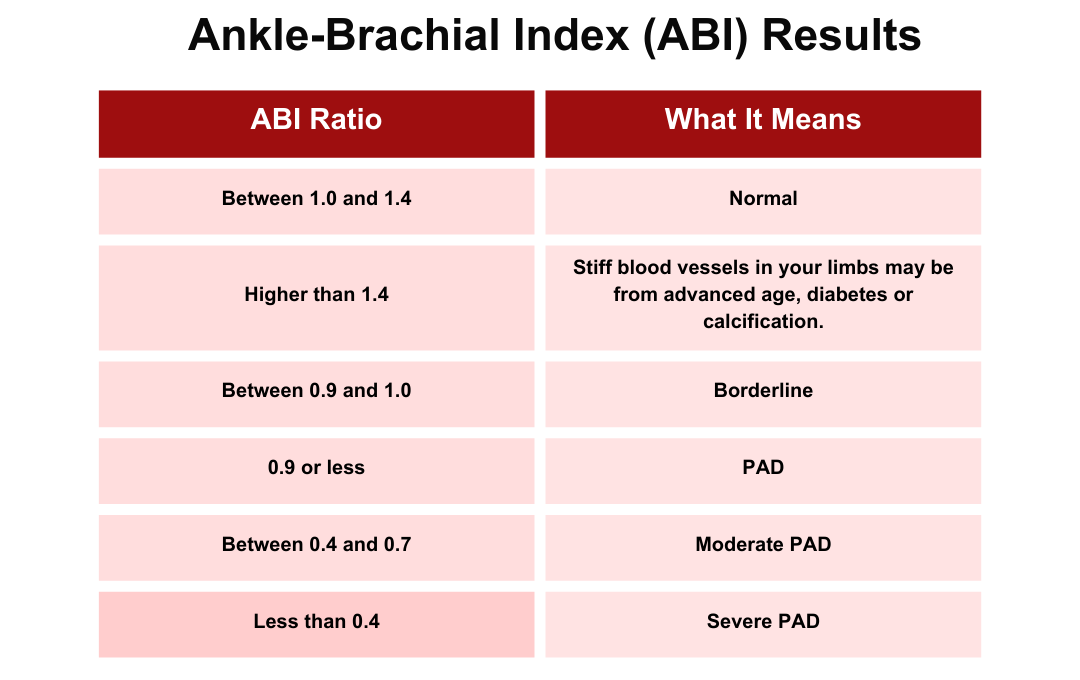
A common method for diagnosing peripheral artery disease (PAD) is the ankle-brachial index (ABI) test. This quick, non-invasive procedure measures blood pressure in your ankle and compares it to the pressure in your arm. A medical professional uses a standard blood pressure cuff and a specialized ultrasound device to assess blood flow and identify indicators of PAD. You might be asked to walk on a treadmill, allowing for measurements to be taken both before and after physical activity.
If you have a high or low ABI, your doctor may order more tests to check for PAD or other problems.
A normal ankle-brachial index (ABI) is 0.9 to 1.3. Lower values suggest peripheral artery disease (PAD), with 0.41-0.90 indicating mild to moderate PAD and 0.7 or less significant PAD. However, diabetics and those with chronic kidney disease may have falsely high ABIs (1.3 or more) due to stiff arteries.
Ultrasound
Ultrasound imaging uses sound waves to visualize internal body structures. A handheld instrument, known as a transducer or probe, is positioned on the skin’s surface, enabling a physician or technician to examine your arteries, assess blood flow, and identify any blockages requiring immediate attention.
Angiography or Angiogram
Angiography is another technique to detect artery blockages. It uses a dye or a contrast material injected into the blood vessels to allow the doctor to view the blood flow as it happens. The flow of dye is visible with the help of X-ray imaging techniques, such as magnetic resonance angiography (MRA) or computerized tomography angiography (CTA). This is useful to determine the location, type, and extent of blockage in the artery.
PAD Treatments
To streamline treatment, minimally invasive treatments for PAD, such as angioplasty, stent placement, atherectomy, or a combination, can be performed immediately following diagnosis when clinically appropriate.
Angioplasty involves inserting a catheter with a thin guidewire and a balloon-tipped device. The balloon is inflated at the blockage to compress the plaque against the artery wall, then deflated and removed, leaving the guidewire in place.
Stent placement typically accompanies angioplasty (a procedure called stent angioplasty). A stent, a small expandable mesh tube, is inserted and deployed at the narrowed area to keep the artery open and improve blood flow.
Atherectomy may be performed before angioplasty or stenting. This procedure uses a catheter with a small blade or laser at its tip to physically remove plaque.
If you have questions about any of these treatments or pre and post-procedure preparations, ask your vascular specialist during your evaluation.
PAD Management
Management of PAD in patients with intermittent claudication should focus on risk factor modifications such as tobacco cessation, controlling blood sugar, high blood pressure, and aspirin therapy whenever indicated.
PAD patients have a higher risk of stroke or a heart attack. The presence of PAD in patients with coronary arterial disease (CAD) is associated with adverse cardiovascular outcomes and progressive atherosclerosis. Improved PAD detection is crucial for effective cardiovascular prevention and treatment.
Schedule Your Appointment with a Specialist
Our specialists at USA Vascular Centers can discuss your PAD complications and PAD symptoms and suggest the best course for PAD treatment based on your specific medical condition. All of our locations are accredited by the Accreditation Association of Ambulatory Health Care (AAAHC), which means that our doctors constantly meet and exceed the highest standards of patient care.
To schedule your appointment with one of our specialists, please call us at 888-773-2193 or schedule online.
Frequently Asked Questions
What is asymptomatic PAD?
PAD can exist without noticeable symptoms and continue to progress, making it a “silent” threat.
Why is asymptomatic PAD dangerous?
Even without symptoms, PAD can progress and lead to serious complications like heart attack, stroke, and critical limb ischemia (CLI).
Who is at risk for asymptomatic PAD?
Individuals who smoke, have diabetes, high blood pressure, high cholesterol, are over the age of 50, and have a family history of PAD or heart disease are at a higher risk for developing asymptomatic PAD.
How is asymptomatic PAD diagnosed?
Asymptomatic PAD can be diagnosed through vascular screenings or diagnostic tests such as the ankle-brachial index, ultrasound, or MRI.
How can I prevent PAD, even if I’m currently asymptomatic?
To reduce the risk for asymptomatic PAD or manage PAD symptoms, it is important to make lifestyle modifications such as quitting smoking, managing diabetes, controlling blood pressure and cholesterol, regular exercise, and maintaining a healthy diet.