Peripheral artery disease (PAD) can lead to noticeable skin changes, such as shiny skin, discoloration, rashes or wounds that don’t heal. These symptoms are often early warning signs of peripheral artery disease and should be examined by a vascular specialist for an accurate diagnosis. While PAD cannot be cured, non-surgical treatments are available that can bring relief to painful and uncomfortable symptoms.
How Does PAD Affect Skin?
Peripheral artery disease is caused by atherosclerosis, a narrowing or blockage of arteries caused by plaque buildup. This limits blood flow to the lower extremities, making even simple activities like walking and exercising difficult. If left untreated, PAD can increase your risk for heart attack, stroke, and even limb amputation.
Peripheral artery disease can also affect the skin in different ways. Some individuals may notice leg discoloration, while others may experience shiny skin or poor leg hair growth. In severe cases, arterial ulcers (open, non-healing wounds) may develop, leading to severe infection.
What Skin Changes Are Associated With PAD?
When plaque builds up in your arteries, it restricts blood flow and impacts circulation. This can lead to discoloration, changes in skin texture, and other complications. Some common peripheral artery disease skin changes include:
Color Changes
Purple, pale, or bluish discoloration on the lower extremities is called cyanosis. This occurs when oxygenated blood is not reaching the tissue, causing skin discoloration. If the skin appears dark purple or black, it could be a sign of tissue death or severe PAD progression.
Texture Changes
Some PAD patients experience changes in skin texture, like shiny legs, dry skin, and scaling. This is caused by poor circulation and restricted blood supply. Reduced blood flow caused by PAD can also affect hair follicles, decreasing leg hair growth.
Wounds and Sores
In extreme cases, PAD can cause slow-healing wounds and sores caused by arterial ulcers. This is a common symptom of critical limb ischemia (CLI), a more progressive stage of PAD. Poor circulation and blood flow can also lead to skin infections and, in severe cases, gangrene. Gangrene can be caused by a chronic disease that harms the circulatory system when blood supply to certain tissues is stopped.
Contact a vascular specialist immediately if you experience any of the above skin issues. Specialists at USA Vascular Centers can evaluate whether your skin changes are due to peripheral artery disease (PAD) or another health condition. If PAD is determined to be the underlying cause, our vascular doctors will recommend the appropriate treatment to address your condition effectively.
Understanding the Severity of PAD-Related Skin Changes
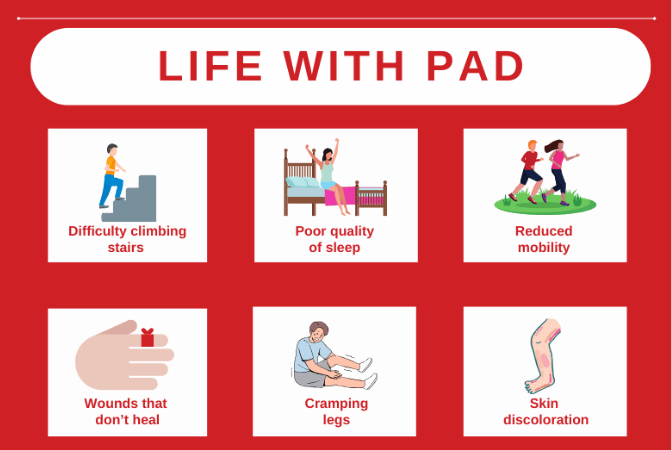
Most peripheral artery disease-lead skin changes are paired with other symptoms that can indicate the severity of the condition.
Mild to Moderate Skin Changes Indicating PAD
Changes in skin texture and discoloration in the legs are often the first signs of PAD. These symptoms develop gradually and may be paired with other common symptoms, such as leg pain and numbness.
These symptoms can slowly start to impact daily life. Over time, dry, scaly skin could become itchy and uncomfortable, and hair loss might be more prominent than before. If you recognize these early signs, schedule a consultation with a vascular specialist for an accurate diagnosis.
Advanced Skin Changes Indicating PAD
If these warning signs are ignored, it could lead to reduced blood flow and a higher risk of severe pain or discomfort. Skin texture and color changes can lead to ulcers or non-healing wounds, increasing the risk of infection.
If you’re experiencing severe pain, dark purple discoloration, or arterial ulcers, seek immediate medical attention to prevent further tissue damage.
Don’t let peripheral artery disease (PAD) sneak up on you. Take our quick risk assessment quiz and discover your risk for developing PAD.
How to Treat Skin Changes from Peripheral Artery Disease
Peripheral artery disease skin changes should always be evaluated by a qualified vascular specialist. During a vascular evaluation, non-invasive tests like the ankle-brachial index (ABI) and ultrasounds are used for diagnosis.
High-risk patients, including those with a history of smoking, diabetes, high blood pressure, high cholesterol, or a family history of vascular disease, should consider regular vascular screenings. Early detection through these screenings can help diagnose and manage PAD effectively to reduce the risk of complications.
If you are diagnosed with PAD, the experienced specialists at USA Vascular Centers will develop a treatment plan that can help decrease your pain and restore blood flow to the affected areas. Depending on your condition, the following treatments may be recommended:
- Angioplasty: A small balloon opens narrowed arteries and improves blood flow.
- Angioplasty with stent placement: After a balloon angioplasty, a stent is placed inside of the artery to keep it open and prevent future build-ups.
- Atherectomy: A blade or laser carefully removes plaque from the artery’s walls.
At USA Vascular Centers, we specialize in performing non-surgical, outpatient PAD treatment. Our treatments do not require general anesthesia, a hospital stay, or a lengthy recovery. After the treatment, patients can recover from the comfort of their own homes.
We accept most insurance plans, including Medicare and some Medicaid plans. You can verify your insurance when you schedule online or call our office at 888.773.2193.
Schedule a Consultation at USA Vascular Centers
USA Vascular Centers is dedicated to diagnosing and addressing peripheral artery disease (PAD) and its associated skin changes. With our nationwide network of outpatient medical centers, we make advanced, minimally invasive PAD treatments accessible and convenient.
To get started on your journey towards better vascular health, schedule online today or call 888.773.2193 to speak with a member of our Care Team.
How do I know if my skin changes are related to PAD?
Shiny skin, discoloration, or non-healing sores paired with leg pain or numbness may be PAD-related. Consult a vascular specialist for an evaluation and accurate diagnosis.
Can PAD-related skin issues lead to infections?
Yes, skin issues related to peripheral artery disease can increase your risk of infections and lead to slow-healing wounds and arterial ulcers.
Is there a cure for PAD-related skin changes?
PAD is a progressive disease that cannot be cured. However, early diagnosis and treatment can effectively help manage symptoms and prevent further complications.
How often should I get screened if I have PAD symptoms?
Schedule a vascular screening if you notice symptoms like skin changes or discoloration. High-risk patients who are over the age of 50, overweight, or have diabetes should also have annual vascular screenings.