The prevalence of vascular conditions in the United States is quite surprising. It’s expected that 1 in every 20 Americans over 50 suffer from peripheral artery disease (PAD).¹ If you have any of the PAD risk factors or have any of the symptoms, schedule an appointment with a vascular doctor immediately to get a diagnosis and discuss treatment.
During the consultation, you may find that your doctor uses the terms PAD and PVD. This can be confusing. PAD stands for peripheral artery disease, while PVD is the abbreviation for peripheral vascular disease. Although there are similarities, both terms cannot be used interchangeably, and there are slight differences in each condition. Here’s everything you need to know:
Understanding The Differences Between PAD vs. PVD
With a quick search, you’ll find that the terms PAD vs. PVD are sometimes referred to as the same condition. However, while PAD may always be PVD, PVD isn’t always PAD.
Peripheral vascular disease (PVD) is an overarching term for different vascular diseases that result from circulatory dysfunction caused by damage to arteries or veins. The symptoms and risk factors are similar, so it’s important to understand the differences between PAD and PVD and get diagnosed by a medical professional.
At USA Vascular Centers, our vascular doctors specialize in diagnosing and treating PAD in the lower extremities. Our specialists can help you determine if you’re suffering from PVD or PAD and recommend a personalized treatment plan to improve your condition and quality of life.
What is Peripheral Vascular Disease (PVD)?
Peripheral vascular disease (PVD) is a slow and progressive disease that impacts the blood vessels in the body outside the heart. Conditions that block blood flow through a vessel, whether an artery or a vein, are classified as peripheral vascular disease. Patients at higher risk for developing PVD are patients who currently have:
- Peripheral artery disease (PAD)
- Chronic venous insufficiency (CVI)
- Deep vein thrombosis (DVT)
- Coronary artery disease (CAD)
It’s important to note that just because you have one of these conditions, it doesn’t necessarily mean you have PVD. It’s best to schedule a consultation with your medical provider for a true diagnosis of your condition.
Peripheral Vascular disease (PVD) is diagnosed and treated by first determining the underlying cause. The American Heart Association categorizes PVD into two types: functional and organic.
- Functional PVD occurs when blood vessels are compressed or spasm. Chronic venous insufficiency (CVI) is the most common form of functional PVD.
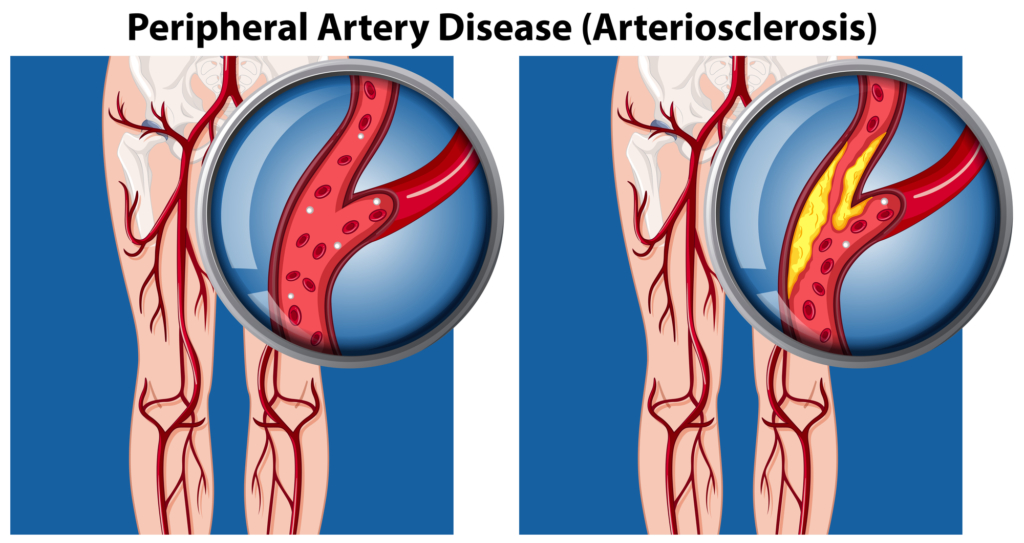
- Organic PVD refers to the blockage of blood vessels, most commonly caused by atherosclerosis. Atherosclerosis is a build-up of fat, cholesterol, and other substances in the bloodstream that causes narrowing of the arteries or blockages. Peripheral artery disease (PAD) is primarily caused by atherosclerosis, which means it is a type of organic PVD.
What is Peripheral Artery Disease (PAD)?
Peripheral artery disease (PAD) is caused by plaque deposits in the arteries. When plaque builds up, it makes it more challenging for the arteries to carry blood, oxygen, and nutrients to the legs. PAD and PVD are both considered progressive diseases. If too much plaque accumulates over time, it can completely block the artery and cut off circulation.
PAD cannot be reversed. There are minimally invasive treatments that can help lessen the impact of PAD symptoms. If you show any signs or symptoms of PAD, schedule an appointment with a vascular doctor.
JOIN OUR NEWSLETTER FOR HEALTH TIPS
Key Similarities between PAD vs. PVD
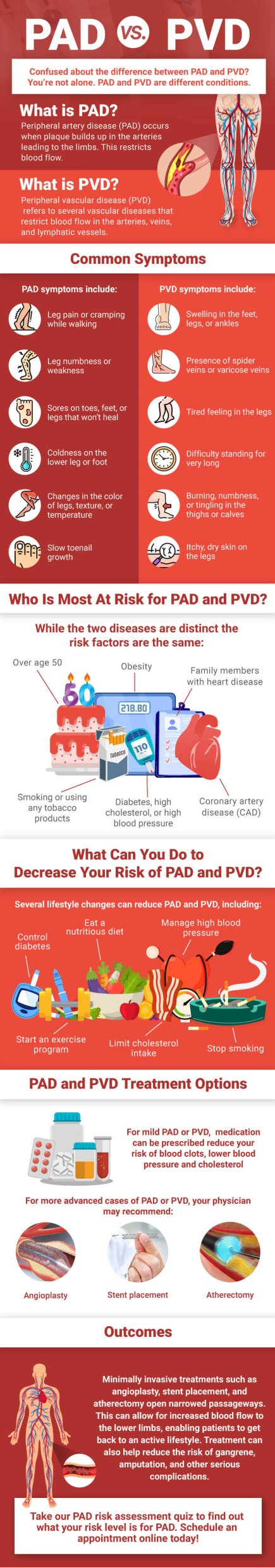
The main similarities between PVD vs. PAD are the symptoms and risk factors. Individuals with either condition may experience leg pain, numbness, or cramping. Other common symptoms include:
- Tingling in the feet
- Pain in the legs when exercising
- Sores that won’t heal
Some of the common risk factors of both PVD and PAD include:
- Smoking
- Diabetes
- High blood pressure
- High cholesterol
- Being over the age of 50
If you have any of these symptoms and suspect a serious vascular condition, the first step is to schedule an appointment with a vascular doctor. They’ll be able to diagnose your condition and offer treatment plans that align with the severity of your disease.
Key Differences between PAD vs. PVD
Peripheral arterial disease (PAD) is a type of PVD that most commonly affects the lower extremities. However, PAD afflicts only the arteries, while PVD may affect any blood vessel outside of the heart, including veins and lymphatic vessels. This means conditions like CVI and DVT can be considered PVD as well.
While there are some overlapping symptoms and signs, there are also some key differences. Here’s how they compare:
| PAD | PVD |
| Claudication: Pain or cramping in legs (muscles calf, thigh, or buttocks) during activity, which disappears at rest. | Swelling in the legs, ankles, or feet |
| Skin changes: While reddish-blue discoloration can occur, it’s not as common as other changes. | Thin, brittle, shiny skin on the legs and feet. Decreased skin temperature |
| Slow healing or non-healing sores (ulcers) on toes, feet, or legs | Varicose or spider veins |
| Loss of hair on legs | Itchy, dry skin on your legs |
| Poor toenail growth | Tired or achy legs |
| Erectile dysfunction | Burning sensation in the calf or thigh |
| Leg or foot that feels cool or cold to the touch compared to the other leg | Difficulty standing for long periods of time |
Treatment Options For Your Condition
A doctor may recommend several treatment options for PVD, including medication to improve blood flow or dilate the blood vessels. For more advanced cases, minimally invasive treatments may be recommended.
While the team at USA Vascular Centers doesn’t treat all types of peripheral vascular disease (PVD), we can help you access minimally invasive treatments for PAD. We have a national network of outpatient centers dedicated to providing non-surgical treatments for PAD in the lower extremities.
The first step you’ll need to take is to get diagnosed. To accurately diagnose PAD, a vascular doctor may ask about your symptoms and medical history and perform a physical exam. An ankle-brachial test (ABI) is an initial diagnostic test for PAD, which measures the blood pressure at your ankle compared to that in your arm. If your vascular doctor believes you would benefit from treatment, they may recommend one of the following:
Our vascular doctors specialize in the following procedures:
- Angioplasty: a balloon is inserted into the affected artery and inflated to compress the plaque buildup against the walls.
- Stent placement: a wire mesh is inserted into the artery to increase blood flow.
- Atherectomy: a tiny catheter is inserted with a blade on the tip to scrape away plaque.
Schedule Your Consultation with USA Vascular Centers Today
If you’re suffering from peripheral artery disease, the best way to understand your condition and available treatment options is to seek a consultation with a vascular specialist. The vascular doctors at USA Vascular Centers have expertise in diagnosing PAD and performing minimally invasive procedures that can alleviate symptoms and improve your quality of life.
Schedule a consultation or call us at 888.773.2193 to start on your treatment journey at one of our centers nationwide.
Sources Cited
- U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES, National Institutes of Health, & National Heart, Lung, and Blood Institute. (n.d.-c). Facts about Peripheral Arterial Disease (P.A.D.). In the National Institutes of Health.